COMMON PROBLEMS & DISEASES
Information about common child problems, including tips on home management, self-care, and when to contact a doctor.
Can Oral Rehydration Salts ORS be used for everyone?
ORS is an abbreviation for oral rehydration solution. Whatever we intake in our body,it should be balanced. Ample quantity of water advised is 8 to 10 glasses in a day, if we take more than advised quantity, our kidneys will have to work more than usual and it may affect its smooth functioning. On the other hand if the intake is less it would lead to dehydration further leading to suboptimal working of kidneys.
ORS is safe and can be used to treat anyone suffering from diarrhoea/dehydration, without having to make a detailed diagnosis before the solution is given. It is also safe for infants on breast milk, however, feeding must also be continued.ORS is extremely cost-effective. Compared to traditional IV therapy, ORS costs just a few rupees. This makes ORS much easier to deploy in major humanitarian crises and more patients are able to be treated. Additionally, ORS can be formulated and administered at home as soon as symptoms appear. Instead of going to a hospital for IV treatment, which may already be difficult for patients in developing countries, rehydration can begin right away. ORS is non-invasive i.e. it doesn’t require needles, or pricks, which can lead to infection if not administered properly. Plus, it doesn’t require guidance to administer.
However, if we take ORS on daily basis, it will affect our normal balance of sodium in the body which may lead to malfunctioning of our system up to a certain extent.ORS is comprised of Sodium chloride(salt),Potassium chloride,Sodium bicarbonate,glucose, etc. which clearly suggests that sodium intake is going to be more than usual. Excessive amount of any element in your blood is never good for our health.
ORS is useful when we are suffering from diarrhoea which renders us dehydrated. Loss of water can be overcome when we drink ORS mixed water. There are very rare side effects thoughe.g.gas,bloated abdomen,etc.Drinking ORS on daily basis,I personally feel is notgood for our body. Drink clean water and fresh juices that will be anytime good. Avoid carbonated drinks.
Happy & Healthy Living!!!
Why is breast milk better than formula?
Choosing whether to breastfeed or formula feed their baby is one of the biggest decisions expectant and new parents will make. Health experts agree that breastfeeding is the healthiest option for both mom and baby. It is recommend that babies feed only on breast milk for the first 6 months. Thereafter breast milk must be continued as a main part of their diet until they are at least 1to 2 years old.
Breastfeeding is a wonderful way to bond with your little one. Here are some of the many other benefits of breastfeeding:
- Breast milk naturally has all the nutrients babies need to grow and develop.
- Breast milk has antibodies that can help prevent your baby from getting sick.
- Breastfeeding can help prevent health problems in your baby, such as allergies, eczema, ear infections, and stomach problems.
- Breastfed babies are less likely to be hospitalized with breathing infections.
- Breastfed babies are less likely to become obese or have diabetes.
- Breastfeeding may help prevent sudden infant death syndrome (SIDS).
- Mothers who breastfeed find it easier to lose weight after pregnancy.
- Breastfeeding may help lower the risk for breast and ovarian cancers, diabetes, and certain other diseases in mothers.
It is true that breastfeeding is not always easy and natural for moms and babies. It may take some time for both mother and baby to get the hang of it. Skin to skin contact at birth will help mother and baby get a good start with breastfeeding.Being a new parent takes time, and feeding is no exception to this rule.It is important to note that mothers do not need to follow a special diet while breastfeeding. It is rare that a baby will seem sensitive to certain foods, like spicy or gassy foods such as cabbage. There are very few health problems that make breastfeeding not possible which are as follows –
- Mothers with HIV or AIDS, as they can pass the virus to their baby.
- Mothers on certain medicines needed to treat ongoing health problem.
- Mothers with an alcohol or drug addiction.
There are other reasons women are unable to breastfeed, but with good support and knowledge, most of these can be overcome.The decision about how to feed your baby is a personal.
Should I massage my baby every day?
The age-old tradition of massaging babies has many advantages for both babies and mothers. It is a highly prevalent practice in Indian society that it has been passed from mother to daughter and generations. It is a great way to express your love, care, and affection for your baby. A massage can soothe the baby and help him stay relaxed
And comfortable. It also helps the baby to sleep better and cry less. The gentle, rhythmic, and soothing strokes of your hands during a massage stimulate the production of the hormone oxytocin in you and your baby. Oxytocin is the hormone that gives you that warm, loving feeling when you hold your baby close or breastfeed her.
Babies love routines and repetition, so if you massage your baby, in the same way, every time, she will learn what to expect and enjoy her massage all the more. Start your baby’s massage with her feet and work your way up the body finishing with her head. Legs are a good place to start a massage because your baby is used to having her legs touched during nappy changes. Coconut oil or cream can be used however you should warm the oil or cream by rubbing it between your palms. Massage should be started with thighs to toes in a milking movement. The same pattern should be followed for arms starting from shoulders to fingers. For your baby’s chest and tummy, do circular clockwise movements. The circular movements on her tummy, done with gentle pressure, can help move things along her digestive tract. Mothers should also gently push their knees into their tummy by holding the baby’s legs below her knees. This will help her pass trapped gas.
In India, no baby massage is complete without a head massage. But some babies like having their heads touched more than others. You need to be very gentle with your newborn’s head as her skull bones will not have fused yet. These are called the fontanelles. There are two fontanelles, a larger one on the top and a smaller one at the back of your baby’s head. The back fontanelle closes by the time your baby is about6 weeks old but the fontanelle at the top of your baby’s head only closes by the time
she is about 18 months old. For the first six weeks, do not apply any pressure while giving your baby a head massage. Just pat the oil gently onto all parts of the head and let the oil soak in on its own. Once your baby’s head hardens, you can gently press with your fingers in small circular movements as you move around your baby’s head. But never apply pressure to the top of your baby’s head where the larger fontanelle is still soft.
As long as your baby cannot hold her own head up, put the oil on her head while she is lying on her back. This way any oil that drips will fall back and not onto her face. Once your baby holds her head up, you can apply oil to her head when she lies on her tummy.
If your baby has a cradle cap, do not pick at it while applying the oil. You will find that if you let the oil sit on your baby’s head overnight, it will help to soften the crust, which should then fall off on its own during the bath or while washing or combing your baby’s hair afterward. Even if it doesn’t, the cradle cap doesn’t disturb your baby and is very common. It often goes away on its own as your baby grows.
If your baby has a rash, do not apply any oil or cream to your baby’s skin without first checking with her doctor. If you feel that the rash is caused by the oil or cream you have been using to massage your baby, stop using it and consult her doctor to get advice on which oils or creams will suit the baby.
Some experts say it is better not to massage your baby if she has a fever or is unwell. But others say that a gentle massage during a viral might help soothe body aches. If your baby has a fever, take advice from your doctor before giving her a massage. If your baby’s fever is rising, she might feel cold. So you can just rub and stroke her over her clothes, without undressing her. On the other hand, if her fever is coming down, she might feel hot and prefer to remove her clothes. Observe your baby and try to see what makes her most comfortable. In winter, you can give your baby a massage. But she will enjoy it only if she doesn’t feel cold. So make sure the room is comfortably warm before undressing her.
Is hepatitis B vaccine necessary at birth?
Its hard to imagine putting your newborn through the pain of a prick shot, but a little stick early in life is an important first step in protecting the baby against a deadly disease. All babies should get the first shot of the hepatitis B vaccine before they leave the hospital. This shot acts as a safety net, reducing the risk of getting the disease from moms or family members who may not know that they are infected with hepatitis B.
What is hepatitis B ?
Hepatitis B is a serious contagious disease caused by the hepatitis B virus. The virus if enters the bloodstream attacks the liver, and causes serious damage. When babies get infected, the virus usually remains in the body for a lifetime (this is called chronic hepatitis B). About 1 out of 4 infected babies will die of liver failure or liver cancer as adults.
Babies and children can get hepatitis B in the following ways:
- At birth from their infected mother
- Being bitten by an infected person
- By touching open cuts or sores of an infected person
- Through sharing toothbrushes or other personal items used by an infected person
- From food that was chewed (for a baby) by an infected person
The virus can live on objects for 7 days or more. Even if you don’t see any blood, there could be a virus on an object.
Is it serious? Is there a cure for hepatitis B?
It can be life-threatening. Although there are several medicines to help people who have life-long hepatitis B virus infection, there is no medicine that “cures” it. The good news is that hepatitis B can be prevented by vaccination.
Why does my baby need a hepatitis B shot at birth?
Medical groups such as the American Academy of Pediatrics, The American Academy of Family Physicians, The American College of Obstetrician and Gynecologists, and the Centre for Disease Control and Prevention recommend that every baby get the hepatitis B vaccine at birth, before leaving the hospital. It is important to vaccinate babies at birth so that they will be protected as early as possible from any exposure to the hepatitis B virus. A baby who gets infected with the hepatitis B virus during the first five years of life has a 15% to 25% risk for premature death from liver disease, including liver failure or liver cancer.
When a mother has hepatitis B the baby requires an additional shot of hepatitis B immunoglobulin (HBIG) in addition to normal vaccination. HBIG works best if it is given in the first 12hrs of birth.
Schedule, Safety, and side effects
The recommended schedule consists of 3 doses at birth, 1 month, and 6 months respectively. The vaccine is safe. The only side effect documented is mild fever (up to 101oF) and pain at the site of administration.
Thus, it is highly recommended for all babies.
Malaria in Babies - Causes of Malaria in Baby
Historical background
The name “malaria” (meaning bad air in Italian) dates back its origin in 1740 when it was first used by H. Walpole while describing the disease. Later in 1889 Sir Ronald Ross discovered that mosquitoes transmit malaria.
What is malaria?
It is a common mosquito-borne disease, characterised by fever, chills, sweating fatigue, anaemia and enlarged spleen. It can be a serious illness in babies and young children.
How common is malaria in India?Is malaria seasonal?
Malaria is widespread in India, most common in Maharashtra, Orissa, Chhattisgarh, Madhya Pradesh and Jharkhand. About 2.5 million malaria cases are reported in South Asia each year. Three quarters of these cases come from India.It occurs all year round, but the number of cases does shoot up during and just after the monsoon season. This is because warm humid weather and stagnant water provide a perfect breeding ground for mosquitoes.
How does malaria spread in babies?
It is caused by Plasmodium parasites. There are four different stains (plasmodium vivax, plasmodium falciparum, plasmodiumovale, and plasmodium malaria). P falciparum and vivax are common in India. It is spread by the bite of an infected Anopheles mosquito. The mosquitoes that carry malaria usually bite at night, unlike the mosquitoes that carry dengue or chikungunya that bites during day time. It can also be transmitted through an infected blood transfusion and from the mother to the baby before delivery (congenital malaria).
What are the symptoms of malaria in babies?
Symptoms usually appear at about eight days to three weeks after the infection. These include –
- Fever
- Shivering
- Cough and cold
- Irritability and drowsiness
- Poor appetite
- Diarrhoea, often with green stools
- Sleeplessness
- vomiting
- Stomach pain
- Some young children have a low body temperature (hypothermia) instead of a fever
- Seizures
What to do if the baby has symptoms of malaria?
Most of the symptoms are common to flu, dengue, and chikungunya, first step here would be to seek medical advice. If malaria is diagnosed then the baby requires the following-
- Plenty of fluids/rest
- Nutrition
- Medicines to reduce fever
- Antimalarial drugs depending on the type of malaria
If the disease is severe the baby needs to be hospitalized for intravenous drugs and fluids. A child with malaria may be ill for about 7 to 10 days
How to reduce the risk of catching malaria?
As mosquitoes cause this disease, it is important to keep mosquitoes at bay. This can be achieved by
- keeping home and surroundings free of mosquito breeding grounds(stagnant water).
- Removing empty containers or old flowerpots where water can collect.
- Adding a few drops of kerosene oil to coolers, open drains, small ponds, and other places where water tends to collect
- Other measures include – light clothing as dark color attracts mosquito, wearing long sleeves
- Using age-appropriate mosquito repellent and mosquito nets while sleeping
Despite being preventable it threatens the lives of about 3.3 billion people around the world. High maternal mortality, low birth weight and maternal anemia are also consequences of this devastating disease. To conclude the prime focus should be the prevention of the disease as we all know “Prevention is better than cure.”
Sunscreen can leads to overheating and dehydration in new born
With Summers coming up the most common query of parents of newborns and infants is how to enjoy being outdoors without allowing the baby to get sunburned. The most common answer that they get and assume is “Sunscreens”.
However, up to 1999 the AAP (American Academy of Paediatrics) strictly condemned the use of sunscreen lotions in babies who are less than 6 months old. Thereafter a slight modification in the recommendation is made. It now advocates the use of small amounts of SPF 15 sunscreens that can be applied to the areas which are directly exposed to the Sun and cannot be covered with clothing, such as the face and back of hands. However, the use should be restricted and kept as minimal as possible. There is still a lack of data supporting the use of sunscreens in babies less than 6 months of age also it cannot be conclusively commented that the benefits of avoiding sunburns outweigh the risks associated with sunscreens.
Sunscreens also contain certain chemicals which can be harmful to premature baby skin. Sunscreens with para-aminobenzoic acid (PABA) must be avoided, it can lead to itching redness, and rash. Other chemicals which must be looked for and avoided are benzophenones like dioxybenzone, oxybenzone, or sulisobenzone, and homosalate, octy-methoxycinnamate (octinoxate), and parabens (butyl-, ethyl-, methyl-, and propyl-). These chemicals can affect the development of brain and reproductive organs.
Young Babies can’t regulate body temperature, this makes them prone to overheating and dehydration, thus FDA (Food and drug authority) had laid down certain guidelines which are as follows –
- Parents need to keep infants and babies out of the sun as much as possible.
- If in case the infants need to go outside, the sun must be avoided when ultraviolet rays are strongest i.e. between 10 a.m. and 3 p.m.
- Parents can create a canopy over the baby’s carrier or stroller.
- The babies must be dressed in lightweight, tight-weave long pants; a full-sleeve shirt and a wide-brimmed hat
- The parents must watch carefully for signs of overheating and dehydration (Nonpassage of urine).
- The baby must be given breast milk or formula regularly.
- In case the baby develops a sunburn, the baby must be moved out of the sun immediately, and a cold compress should be applied as soon as possible.
- Lastly, parents should try to limit outdoor activity to 30 minutes.
Sometimes, even with the best of intentions, a baby/newborn/infant may get sunburned. Usually, this is because of light. This can be relieved with the use of cold compressions. However, if the burn is severe, it will require medical attention, so be sure to contact your paediatrician if your baby becomes sunburned.
How jaundice at birth can be prevented (A simple advisory for mothers)
Jaundice, or hyperbilirubinemia, is a common medical condition that develops in newborns within the first two to five days of life. It occurs due to high levels of bilirubin, which is a waste product from the breakdown of haem-containing proteins presents particularly in red blood cells. It is excreted from the body by the liver, in urine, and in stool. The life span of newborn red blood cells is less compared to the adults, further, the liver is immature to handle the increased bilirubin load. This results in an imbalance between bilirubin production and excretion leading to jaundice.
There is no sure way to completely prevent jaundice, knowing risk factors may help to determine what can be done to prevent and prepare for newborn jaundice. However, the various steps that one can take care are as follows –
- Identifying risk factors –Certain blood incompatibilities can cause more blood to break down, producing more bilirubin such as –
- Mothers with Rh negative and O+ blood group
- Genetic enzyme deficiencies, like glucose-6-phosphate dehydrogenase deficiency
- Reducing the risk of preterm birth – Babies born before 37 weeks are at an increased risk of developing jaundice. The liver of a preterm baby is less developed than that of a full-term baby, making it even more difficult to eliminate bilirubin. Some pre-term risk factors, such as age or multiple births, cannot be remedied. Many environmental risks can be –
- Early and consistent prenatal care can ensure that the baby stays as healthy as possible during the pregnancy
- Chemical contaminants such as tobacco, alcohol, street drugs, and some medications can increase your chances of preterm birth hence be avoided
- Stress is also a major risk for preterm birth hence avoided
- Begin breastfeeding early – It is seen that mothers who begin breastfeeding within the first few hours after birth are more likely to succeed than those who wait. Moreover, the colostrum a mother produces early prompts the baby’s digestive system to eliminate waste, which helped to expel excess bilirubin from the intestines.
- Feeding the baby frequently – A steady supply of milk helps in increasing the baby’s weight and development, including the development of the liver. This is true for both breastfed and formula-fed babies. Ideally, newborns should be fed every 2 hours or at least 8 to 12 times a day.
- Exposing the baby to sunlight – Light reacts with bilirubin, changing it into a form that does not need to pass through the liver in order to be expelled, thereby reducing the risk of jaundice. The baby may be exposed naked to sunlight for about 5 minutes once or twice a day. Prolonged exposure must be avoided as it may cause burns. Alternatively, the baby’s bed may be placed near a sunny window with curtains. Curtains and windows filter out many of the UV rays that can cause problems, allowing the baby to take sunlight without burning.
Dengue Fever Symptoms
Dengue fever is caused by an arbovirus, transmitted to humans by the bite of an Aedes mosquito. Four different serotypes of the dengue virus have been identified. Infection with one serotype provides lifelong immunity to that specific serotype, but only partial short-term immunity to the other 3 serotypes. Dengue is mainly an urban disease present in tropical and subtropical regions.
Primary or first infection may be asymptomatic or present as mild dengue fever, subsequent infections are dangerous. The incubation or latent period is of 4-10 days, thereafter illness occurs in three phases, which are described as follows –
- Febrile Phase: marked by high fever 39 – 40 0C accompanied by generalized body aches, rash, and bleeding manifestations. It usually lasts for 2-7 days.
- Critical Phase: marked by a decrease in temperature, it usually occurs between 3rd to 7th
- Recovery Phase: patient improves, vital normalize, gastrointestinal symptoms subside, and appetite improves
WHO has classified dengue according to the severity of symptoms.
- Dengue with warning signs:- it includes fever with two of the following symptoms:-
- Nausea/vomiting
- Rash resembling measles
- Generalized aches
- Bleeding
- Decreased white cell counts
- Dengue with warning signs: marked by the presence of at least one of these signs
- Pain in stomach
- Persistent vomiting
- Bleeding
- Lethargy
- Decrease in platelets
- Severe Dengue: marked by following:
fluid leaks present as the accumulation of fluid around the liver and in the lungs
Weak and rapid pulse
Severe bleeding
Multi-Organ failure
Factors that put you at greater risk of developing dengue fever or a more severe form of the disease include:
- Living or traveling in tropical areas. Being in tropical and subtropical areas increases your risk of exposure to the virus that causes dengue fever. Especially high-risk areas are Southeast Asia, the western Pacific islands, Latin America, and the Caribbean.
- Prior infection with a dengue fever virus. Previous infection with a dengue fever virus increases your risk of having severe symptoms if you’re infected again.
There is no specific medication for the treatment of dengue infection. People who think they have dengue should use analgesics (pain relievers) with acetaminophen and avoid those containing ibuprofen, Naproxen, aspirin or aspirin-containing drugs. They should also rest, drink plenty of fluids to prevent dehydration, avoid mosquito bites while febrile, and consult a physician.
As with dengue, there is no specific medication for DHF. If a clinical diagnosis is made early, a health care provider can effectively treat DHF using fluid replacement therapy. Adequately management of DHF generally requires hospitalization.
Complications of dengue fever
Dengue fever is an acute viral infection characterized by fever. It is caused by a bite from mosquitoes carrying dengue virus. The primary form of Dengue Fever is characterized by a skin rash and a high fever with severe pain in the head and muscles. Other symptoms may include shaking chills, diarrhoea, and vomiting. Bouts of extreme exhaustion may last for months after the initial symptoms
Dengue fever can result in the following complications:
- dengue haemorrhagic fever
- dengue shock syndrome
These two conditions are rare in occasional travelers to endemic areas, being more common in people who live in an area affected by Dengue and have been repeatedly exposed to the virus.
Dengue haemorrhagic fever
Dengue haemorrhagic fever is a potentially fatal complication of dengue that can cause an enlarged liver and, in severe cases, can lead to shock (a sudden drop in blood pressure). This is called dengue shock syndrome.
Symptoms of dengue haemorrhagic fever are the same as those for dengue, but there are sometimes also:
- tiny spots of blood on the skin
- larger patches of blood under the skin
- bleeding from your gums and nose
- a weak pulse and clammy skin
- sweatiness
- a tender abdomen (tummy) and body
- discomfort (malaise)
- loss of appetite
- fatigue (tiredness)
- sore throat and cough
Four different strains of the dengue virus can cause this complication. If you have previously been infected with one strain of dengue and are infected again with a different strain of the virus, this can cause dengue haemorrhagic fever.
Previous immunity (the body’s ability to resist infection) to a different strain of dengue virus plays a role in this serious complication.
You are also at an increased risk of getting dengue hemorrhagic fever if you are female and under 12 years of age.
The main feature of treatment for dengue haemorrhagic fever is keeping the patient’s fluids at the right level to prevent dehydration.
Dengue shock syndrome (DSS)
This is a complication of dengue haemorrhagic fever in which the symptoms above can be accompanied by symptoms of shock.
Symptoms of shock include:
- a sudden drop in blood pressure
- cold, clammy skin
- a weak rapid pulse
- dry mouth
- irregular breathing
- dilated pupils
- reduced flow of urine
Mortality rates can be as high as 40% if this serious complication is not treated. If it is treated, the mortality rate is 1-2%.
If you have any symptoms of dengue, dengue haemorrhagic fever, or dengue shock syndrome, seek immediate medical help to prevent the disease from progressing
How ORS Works
ORS refers to oral rehydration solution a simple but life-saving beverage of water, salt and sugar formulated in the late 1960s by American and Bengali doctors and researchers working in Dhaka, the capital of Bangladesh. Unlike saline intravenous drips to treat severe dehydration from diarrhoea, ORS was cheap, did not require unusual, sterile equipment, and could be made at home. The potential of ORS in poor countries was enormous.
Diarrhoea was also known to Hippocrates (farther of medicine), and elaborate treatment for diarrhoea is provided in the Vedic texts. In rural Mississippi, for example, a mixture of flour and water is recommended, and another folk remedy suggests apple extracts as a binding agent for mild diarrhoea prior to a visit to the paediatrician.
Rapid evacuation of fluids from the body, which can be caused by cholera or diarrhoea diseases, may lead to chronic dehydration and eventually death. Oral Rehydration Salts are a solution of sugars and salts that helps to slow the evacuation of fluids, allowing for the absorption of electrolytes in the intestines.
The scientific way to put it is ORS works because of the Sodium-Glucose Co-Transport System
- The Discovery of intestinal sodium-glucose transport was the biases of the development of oral rehydration solution and was hailed as the most important medical advance of the 20th
- The jejunum (part of the small intestines) contains SGLT-1 transporter proteins(which transport ions).
- If a 2:1 ratio of Na+ and glucose is consumed, SGLT-1 actively transports both across the epithelial wall. Osmotic imbalance is created.
- Water is immediately pulled into the vascular system. Fluid and electrolytes instantly replenished, avoiding most of GI tract. ORS contains this precise ratio of ingredients.
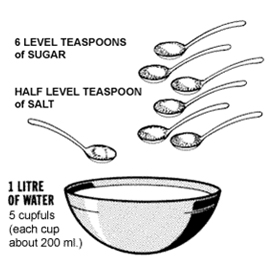
The solution can be made at home too by adding 6 level teaspoons of sugar and 1/2 level teaspoon of salt dissolved in 1 litre of clean water. We need to be very careful to mix the correct amounts. Too much sugar can make the diarrhoea worse. Too much salt can also be extremely harmful. Making the mixture a little too diluted (with more than 1 litre of clean water) is not harmful.
How do I prepare an ORS solution at home for my baby?
ORS is a life-saving solution for babies with dehydration, vomiting, and diarrhoea. It plays a key role in the hydration of babies, however, if not available can be prepared at home with simple steps as discussed below –
How do I prepare an Oral Rehydration salt ORS solution at home? If ORS packets are not available, mix an oral rehydration solution using one of the following recipes; depending on ingredients and container availability:
Recipe for Making a 1 litre ORS solution using Sugar, Salt, and Water
- Clean Water – 1 litre – 5 cupfuls (each cup about 200 ml.)
- Sugar – Six-level teaspoons
- Salt – Half level teaspoon
- Stir the mixture till the sugar dissolves.
The homemade solution is adequate in most causes leading to dehydration. If the diarrhoea is severe, we can buy a special packet of Oral Rehydration Salts. The instructions for preparation are mentioned on the back side of the packet we need to follow them carefully. It is important to note that ORS solution must be given to the conscious dehydrated patient only. It should be given sip by sip every 5 minutes until urination becomes normal. (It’s normal to urinate four or five times a day.) Adults and large children should drink at least 3 quarts or litres of ORS a day until they are well. If the child/adult develops vomiting, we need to continue to drink the ORS. The body will retain some of the fluids and salts we need even though there is vomiting. It’s most important to remember to take sips of liquids slowly. Chilling the ORS may help. In case of diarrhea we need to continue to drink the ORS. The fluids will not increase diarrhea. Someone with symptoms of severe dehydration needs to go to an emergency room or other health care facility to get intravenous fluids (fluids given directly into the veins through a needle). If able to drink, he or she should also drink the ORS. During or after treatment of dehydration, whatever is causing diarrhea, vomiting, or other symptoms should also be treated.
How can you keep your babies from falling sick this monsoon
Monsoons excites the little kid residing in every heart. Splashing in puddles, making paper boats and floating them, and enjoying getting themselves soaked are the things I am sure everybody must have done while growing up. However, the sad part is monsoons bring an onslaught of illnesses that affect our health adversely. Humidity, flooded roads, mosquitoes, water-borne diseases, and dirty and unhygienic environments are all unfortunate parts of this season. Needless to say, kids remain most vulnerable during this season and we should be on our toes to protect them from the vagaries of weather. So below are some useful tips that will help you keep your child fit during the monsoon season.
- Keep your children’s room clean and dry. Maintain normal room temperature and keep their rooms ventilated during the daytime.
- Close all the doors and windows at the evening to prevent mosquitoes and other insects from entering your house.
- Do not switch on ACs in the monsoon as it makes the room temperature low thus providing a perfect breeding ground for mosquitoes.
- Give your child a hot bath during the monsoon. It makes them feel fresh and relaxed.
- Wear dry clothes in the monsoon. Even slightly wet clothing can make your child catch the flu.
- Serve moderately hot food for your child. Avoid eating outside especially roadside food during the season.
Let’s have a look at some of the illnesses kids catch during the monsoon and what you should do to keep your little ones safe.
- Common Cold & Flu
Due to temperature fluctuations during the monsoons can cause nose blockage and headaches. One minute it’s pouring cats and dogs leading tolowering of environmental temperature, within next few minutes we may see sun (higher temperature and humidity)
What Can We Do: Give a healthy diet of fresh fruits and vegetables rich in vitamins, minerals, and antioxidants to boost immunity. We can also supplement multivitamins such as vit. C & E which tend to charge up antibodies to fight the common cold virus.
- Viral Fevers
If the child is having a high fever, chills, or rash, there are chances that he/she may have contracted a viral fever. This is airborne and can be transferred by contact, sneezing, not washing your hands, and sharing food.
What Can You Do: Hand washing plays a key role. Hand sanitizer may be used in case the children are out and unable to wash their hands.
- Malaria
The stagnant water becomes a breeding ground for mosquitos and flies. Dengue, Malaria, and Chikungunya are some of the diseases these mosquito spreads.
What Can You Do: Use mosquito repellents and nets, and wear full-sleeve clothes. Also, try to stay away from dirty puddles and stagnant waters.
Stomach Infection
Every child tends to put his/her hands, toys, and anything else within reach into their mouth. Germs and dirt transfer via this to their little sensitive tummies.
What Can You Do: Kids touch and put everything in their mouths so keep their nails trimmed and clean so that there is no chance of any infection passing to their tummies. Use of liquid hand washes is recommended during this season to prevent the spread of any infection to others.
Despite your best efforts, your children may get sick once in a while, although not as often as if you didn’t take any precautions at all. But getting sick is part of growing up and is the way that your baby’s immune system will learn to fight off infections in the future. However, make sure to take your baby to the doctor if the baby acquires illness.